Common Features
- Conical tip imparts superior tactile feedback
- High flow rate enables faster Cerebro Spinal Fluid (CSF) flashback
- Aggressive anesthetic distribution upon injection
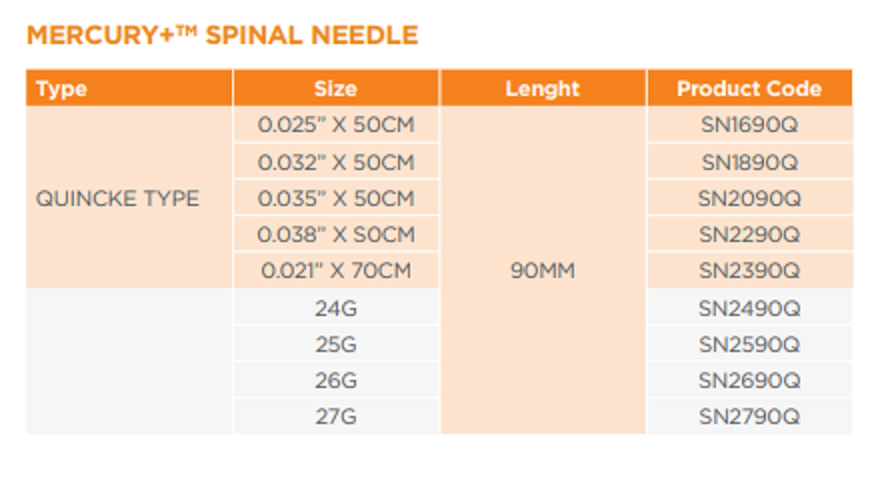
- Sizes: – 16 G to 27 G x 3.5”(90 mm) needle length
Spinal needles vary in their design, usually regarding the tip geometry, but are fundamentally similar and usually come with a stylet and introducer needle. Larger spinal needles may not require an introducer.
Method of use
Spinal needles are used to inject analgesia and/or anaesthetic directly into the CSF usually at a point below the second lumbar vertebra. Spinal needles enter the cerebral spinal fluid (CSF) through the membranes surrounding the spinal cord. An introducer needle is used in some cases to stabilise the insertion of the needle and aid insertion through tough skin. The needle and stylet are advanced towards the dura in the intevertebral space (the stylet stops tissue blocking the needle during insertion). An introducer needle is used in some cases to stabilise the insertion of the needle. Once through the dura and in position, the introducer is removed and the removal of the stylet enables CSF to flow into the needle hub. CSF can be collected for diagnostic purposes or a syringe may be connected to the spinal needle to inject anaesthetic agents or chemotherapy agents.
Whilst Quinke needles tend to cut through the dura (the tough outer membrane), pencil point designs such as the Sprotte and Whitacre are designed to part the fibres of the dura rather than cut them, minimising damage to the dura fibres and reducing the risk of post-dural puncture headaches.
Epidural needles (such as the Tuohy needle) are larger, hollow needles that enter the epidural space. The curve of the needle is designed to enable an inserted cannula to be threaded into the epidural space at an angle. Once the cannula is in place the epidural needle is removed. Anaesthesia and analgesia can be administered via the epidural cannula.